
Impact of COVID-19 on transfusion care of patients with hemoglobin disorders in India
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has posed many unprecedented challenges to the healthcare systems worldwide. The World Health Organization (WHO) declared the COVID-19 pandemic in March 2020. Most countries struggled to contain the infection and treat the infected individuals. Strategies adopted included travel restrictions and lockdowns, resulting in significant challenges for the care of non-COVID patients (1). The reduction in blood donation and challenges in transfusion care were reported by many regions of the world (2-8). A multi-center survey run by the Thalassemia International Federation (TIF), including 42 countries, showed moderate to severe blood shortage during the COVID-19 pandemic, specifically in developing nations, while the impact in western countries was mild to nil despite initial blood shortages (9). The same survey showed a drop in pretransfusion hemoglobin (Hb) levels up to 5g/dL or lower in beta-thalassemia patients in developed countries during the pandemic (9).
In India, patients suffering from chronic illnesses, such as malignancies and Hb disorders, were among the most affected (3,10,11). Aside from travel restrictions, the significant decrease in blood donations made it difficult to receive regular transfusions. A tertiary care institute from India reported a 56% reduction in total transfusion sessions to patients with Hb disorders during the early phases of the pandemic in 2020 (April to June) compared to the same period in 2019 (12). This article aims to provide an overview of the challenges faced by the blood banks and transfusion services in India caring for patients with Hb disorders and the mitigation strategies adopted to overcome them.
The Hb disorders
Hb disorders are broadly classified into two; caused by quantitative defects such as α-thalassemia (α+ α0 thalassemia, Hb H and Hb Bart’s) and β-thalassemia (β thalassemia minor/intermedia/major), and caused by point mutations in the β globin genes, resulting in Hb variants such as sickle cell disease (SCD) (Hb S; S/β thalassemia; Hb S/C), Hb E and Hb D (13,14).
These disorders are prevalent in tropical and subtropical regions of the Mediterranean region, South Africa, South and Southeast Asia, the Middle East, and the Pacific islands (14). With increasing migration, Hb disorders are now seen in more than 71% of countries (14). The 2008 WHO survey estimated that 5.2% of the world population carry a significant Hb variant (Hb S/C/D/E, β thalassemia, α0 thalassemia), with 40% being Hb S trait. In addition, 20% of the world population carries an α+ Hb variant. About 1.1% of couples worldwide are at risk of giving birth to a child carrying a significant Hb disorder, and 3.4% of early mortality (under 5 years of age) is due to Hb disorders (14). SCD is one of the commonest inherited Hb disorders that present with well-described complications such as acute chest syndrome (ACS), vaso-occlusive crisis (VOC), chronic hemolysis, priapism, and stroke (15).
The Hb disorders in India and their burden
Earlier reports reported a 1.2 per 1,000 births (accounting for approximately 32,400 annual births) prevalence rate of significant Hb disorders in India (16). α-thalassemia, β-thalassemia and sickle cell disorders outnumber the other Hb disorders. The average prevalence of α-thalassemia and carriers of β thalassemia is 10–25% and 3–4%, respectively, with a maximum of 1–9% in Maharashtra and Gujrat states (17,18). Several ethnic groups have a much higher prevalence of these disorders due to consanguineous marriage and the natural selection pressure due to malaria prevalence (19,20). Hb S is common in tribes and communities in specific parts of the country with a prevalence rate of 5–35% (17). Hb E is common in the Northeastern states with a carrier frequency of 3–50% (17). Blood transfusion is required as a cornerstone in managing patients with Hb disorders. However, such a huge patient load causes a significant burden on transfusion services in the country.
Blood banks and transfusion services in India and challenges faced during COVID-19 pandemic
Government of India defines a “Blood Centre” as a premise in an organization or institution, authorized for carrying out all or any of the operations including collection, apheresis, processing, storage, and distribution of blood drawn from donors or received from another licensed Blood Centre and for preparation, storage, and distribution of blood components. For this review the term “Blood Centre” and “Blood Bank” are used interchangeably. Blood banks and transfusion services in India have their unique challenges. These challenges were further augmented during the COVID-19 pandemic, besides the new challenges due to the nature of the pandemic (Table 1).
Table 1
| Existing challenges (pre-COVID-19 era) that were augmented during the pandemic |
| Decentralisation of blood establishments/blood banks |
| Non-availability of large pool of voluntary blood donor base |
| Non-availability of centralized component preparation facilities |
| Variabilities in TTID testing methods |
| Lack of adequate/standard transfusion facilities in some hospitals |
| Lack of patient blood management program |
| Unique new challenges during the pandemic |
| Motivating and mobilizing voluntary blood donors |
| Inventory management |
| Consumable and logistic supply chain |
| Ensuring donors and staff safety |
COVID-19, coronavirus disease-19; TTID, transfusion transmitted infectious disease.
Organizational challenges
India has a very diverse and decentralized system of blood establishment/blood bank services, with more than 3,300 blood centers across the country, collecting approximately 12.2 million units annually (21-23). These blood centers function independently and differ in organization type [hospital-based (teaching/non-teaching institutions) or stand-alone] and annual blood collection numbers (from less than 5,000 to as high as >80,000 donations per year). Decentralization has also led to a wide range of quality and performance variations depending on each center’s geography (rural vs. urban) and infrastructure.
Most of the blood transfusion facilities are in either cities or district headquarters, while many far-off rural areas of the country lack blood transfusion services or blood centers with manufacturing facilities. Home transfusions are not practiced in India, limiting this option to patients with Hb disorder. Therefore, visiting a hospital/transfusion center is required to receive a transfusion. With the sudden cessation of routine out-patient care during COVID-19 pandemic, it was difficult for patients with Hb disorders to get their blood transfusions at the required frequency.
Decline of blood donations
Blood centers in India largely depend on replacement or family donations. Due to the lower proportion of voluntary donations, a regular supply of blood and blood components for chronically transfused patients, such as patients with Hb disorders and cancer, is challenging. During the COVID-19 pandemic, the Government of India granted permission to all blood centers (governmental, private, and stand-alone) to organize blood donation campaigns to increase voluntary blood donation in the country. Despite the growth of the recruitment programs for voluntary blood donation during the pandemic, a huge decline in the blood donation rates due to the inherent fear of acquiring the infection during blood donation was reported (4).
Inventory management
Inventory management during the COVID-19 pandemic was very challenging due to the sudden decrease in blood supply. The government allowed the transfer of surplus blood and components from one blood centre to another, but the country’s significant geographical diversity made it difficult. In addition, non-uniform component preparation procedures in different blood collection facilities further complicated inventory management and component distribution. According to the National AIDS Control Organization (NACO) report, 34% (1,131 out of 3,311) of blood centers in India are government-supported and process 78% of the total collection into components such as packed red blood cells, platelet concentrates, and fresh frozen plasma, owing to the limited resources (23).
Variabilities in testing methods on donated blood across the country
Blood donor testing for human immunodeficiency virus (HIV)-1 & -2, hepatitis C virus (HCV), hepatitis B virus (HBV), Malaria, and Syphilis is mandatory in India. However, owing to the decentralization and variable resources, testing methods vary from rapid antigen/antibody tests to enzyme-linked immunosorbent assay (ELISA), chemiluminescence tests, and nucleic acid amplification tests (NAT). Due to this variability, transfusion-transmitted infections (TTIs) have been reported in patients with Hb disorders in India. Many studies from India reported TTI seroprevalence rates in this group of patients of 2.2–5.1%, 1.2–7.4%, and 0–9% for HCV, HBV, and HIV viruses, respectively (24-26).
Blood grouping and cross match methods in India range from manual tube/slide to fully automatic testing. Previous studies reported higher alloimmunization and autoimmunization rates in SCD and thalassemia patients (27-30). The use of immediate spin crossmatch (IgM testing) without screening for rare alloantibodies, may contribute to alloimmunization and hemolytic transfusion reactions.
As most of the reagents used in blood banking in India are manufactured abroad and have a short shelf life, it was very challenging to maintain a regular and adequate supply of testing reagents and consumables during the COVID-19 pandemic due to the lockdowns and restrictions of international flights. In addition, apart from consumables supply, equipment services provided by the vendors for preventive maintenance, calibrations, and repairs were also affected.
Patient blood management program
Patient blood management is a relatively new concept in India and is not universally practiced (31). This resulted from the lack of enough expertise in transfusion medicine and the lack of transfusion medicine under-graduate and post-graduate education and training. Only a few institutions in the country have adequate training facilities for transfusion medicine specialists. Inadequate/inappropriate transfusion is also exacerbated by a lack of national guidelines for the transfusion of patients with Hb disorders. As a result, clinicians order blood based on their knowledge or international standards, which may not apply in our country. However, some centers could adopt patient blood management principles to support the blood requirements during periods of reduced supply, such as starting patients with nutritional anemias on hematinics (32).
Challenges faced for transfusion management of patients with Hb disorders during COVID-19 pandemic
During the pandemic, an advisory from the Ministry of Health and Family Welfare in India instructed states to continue the provision of all essential health services (33). This included blood transfusions for thalassemia and SCD and emergency care. One of the centers in India reported a drop in blood collection to as much as 1/6th to 1/9th when compared to previous years (34). Adaptation to COVID-19 restrictions such as social distancing, staying at home, avoiding non-essential travel, and strict lockdown posed by the government were limiting factors (35). Late presentation of patients to the hospital with life-threatening complications (such as anemia, splenomegaly etc.) due to lockdown and lack of appropriate health care was seen. Some patients feared contracting the virus either during travel or in the hospital (36).
Various factors predispose patients with Hb disorders to infections, such as a history of splenectomy or functional asplenia, oxidative stress due to iron overload, and organ damage, including the adrenal glands (37,38). SCD patients infected with COVID-19 have a higher risk of hospitalization and development of pain and pneumonia as compared to individuals without SCD or trait, although case fatality rates were not significantly different (39).
In a meta-analysis, the incidence of COVID-19 among patients with thalassemia and SCD were 1.34 and 17.22 per 100,000 person-day, respectively and the mortality was around 1.07 per 1,000-day (40). Black SCD patients with COVID had a higher risk of hospitalization, development of pain, and pneumonia as compared to blacks without SCD or trait, although case fatality rates were not significantly different (39).
Mitigating strategies adopted in India during the pandemic
To overcome the challenges in managing these patients, many mitigation strategies were adopted by healthcare centers and transfusion services (Table 2).
Table 2
| Potential challenges | Mitigative strategy adopted |
|---|---|
| Patient blood management | Introduction and application of principles of PBM |
| Use of drugs to reduce the need of transfusions | |
| Revising the transfusion thresholds and policies (wherever possible) | |
| Avoiding iatrogenic blood loss | |
| Clinical care and transfusion | Batching the day care transfusion services (to reduce crowding) |
| Near-home transfusions | |
| Transition to Tele-care | |
| Increasing blood supply | Motivation |
| Social media engagement | |
| Regular call for donors via media | |
| Collaboration with NGOs | |
| Recruitment and travel | |
| Providing travel pass for donors to reach the donation centres | |
| Providing safe transport during lockdowns (by the blood centres for donors) | |
| Providing certificate/photo of donation (for social media promotion) | |
| Tele counselling and screening for basic requirements for blood donations (hence avoiding travel if not eligible) | |
| Voluntary donors register | |
| Maintaining list of donors living in area near the donation centre | |
| Health care workers who are eligible for donation | |
| Donor safety | |
| Pre-registration (for less time in donation centre) | |
| Appointment-based visits to donation centre | |
| Use of Aarogya Setu Mobile App | |
| Screening of donors for temperature upon arrival | |
| Providing masks and hand sanitization | |
| Social distancing in the waiting or donation area | |
| Avoiding outdoor donation campaigns/sessions in crowded area | |
| Rare donor registry | |
| Contacting donors on a case-to-case basis based on the needs | |
| Inventory management | Maintain a buffer stock of additional units (1–2 weeks) |
| Preparation of required components | |
| Considering apheresis platelets collection and use | |
| Demand-based collection and component preparation | |
| Reduce wastage | |
| FIFO policy | |
| Use of ABO compatible units (may not be ABO matched) | |
| Transfer of units to other blood centres | |
| Education of clinicians for appropriate use | |
| Regular audits for appropriate utilization | |
| Consideration of frozen and fractionated blood products | |
| Staff and donor safety | Donor safety |
| Pre-registration (for less time in donation centre) | |
| Appointment-based visits to donation centre | |
| Use of Aarogya Setu Mobile App | |
| Screening of donors for temperature on arrival | |
| Providing mask and hand sanitization | |
| Social distancing in the waiting or donation area | |
| Avoiding outdoor donation campaigns/sessions in crowded area |
PBM, patient blood management; NGO, non-government organizations; FIFO, first-in, first-out.
Patient blood management
Medications
To manage transfusion needs in these patients, many medications were adopted, such as hydroxyurea and Luspartacept. Low dose hydroxyurea therapy (10 mg/kg/day) reduces the need for regular monitoring of blood counts in patients with SCD and thalassemia (41). The role of Luspartacept (erythroid maturation agent) in thalassemia and Voxelator (a Hb stabilizer that prevents Hb S polymerization) in SCD was also explored (42,43). Luspartacept is launched in India but is not routinely used due to its high cost, while Voxelator is not available.
Revised transfusion strategies
Some centers relaxed transfusion thresholds in patients without any cardiac comorbidity to increase the interval between transfusions. As a result of the inability to travel to hospitals and attain proper care, a center reported a median pre-transfusion Hb concentration of 5.8 g/dL (range, 1–8.5 g/dL) for transfusing thalassemia patients, significantly lower than the usual threshold of 9 g/dL for transfusion (12). For SCD patients on chronic automated red cell exchange, a study reported setting of the target hematocrit (Hct) 5% higher (maximum of 36% Hct) at the end of exchange procedure (44).
Avoiding iatrogenic anemia
Reducing the iatrogenic blood loss through the appropriate collection of samples (volume and type vacutainer) was emphasized during the pandemic and played an important role in pediatric patients (45). Elective surgeries were postponed during the pandemic.
Clinical care and transfusion
Batching day-care services
Scheduling fewer patients for transfusions in the daycare was adopted to help maintain adequate social distancing. Appointment slots were prescheduled in batches during the day to ensure adequate staffing. Early communication with blood centers for blood supply and special transfusion needs (e.g., phenotyped red cells and rare blood groups) was practiced (12).
Near-home transfusions
For patients who must travel long distances to reach a transfusion center, arrangements to transfuse patients in local medical centers near their homes helped immensely (46). Logistic support was also provided by many non-governmental organizations (NGOs).
Transitioning to tele-care
Most centers treating patients with Hb disorders have adapted to teleconsultation services to avoid hospital visits except in emergencies (46,47). Telemedicine consults reduce hospital visits and the risk of exposing the patient to potential infections, thus reducing the burden on an already strained healthcare system. During these teleconsultations, advice on regular care, the prevention, and treatment of COVID-19, and dosing of medicines were delivered.
Increasing blood supply
Media campaigns to motivate donors were carried out to overcome blood shortages. Examples were highlighting the blood shortage, the safety of coming to attend blood banks with prior appointments and attending mobile donation campaigns/units near the vicinity of their homes (48). Along with many NGOs, the blood centers provided safe travel options for donors during the travel restriction periods.
Inventory management
Inventory management was one of the most challenging parts, as it involved planning with a high degree of uncertainty. Each blood centre developed its own unique protocol/ plan to maintain a buffer stock depending on the type of medical emergencies or chronically transfused patients they were supporting. The risk of shortage of blood units and the risk of a higher degree of discard due to the cessation of routine surgeries were considered. Actions encouraged included rationalizing the type of components to be prepared (platelets to be made or not) from whole blood donations, use of first-in-first-out (FIFO) policy, considering apheresis platelets collections and considering the options of ABO compatible (non-identical) platelet transfusions.
Conclusions
In conclusion, the COVID-19 pandemic brought up challenges and different mitigation strategies for transfusion care of patients with Hb disorders in India. Maintaining the continuity of blood banks and transfusion services during viral pandemics is vital for this group of patients, among others. Blood banks and transfusion services should develop strategies to maintain blood supply during such pandemics. A team-approach is very important to overcome the challenges faced.
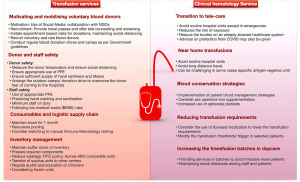
To ensure continuity of care during these challenging times, there is a need for closer communication between the blood center and transfusion services. We summarize here points to consider in facing similar pandemics the future (Figure 1). Local guidelines and policies on the continuity of care of this group of patients in future pandemics are required. Development for patient blood management and home transfusion policies is recommended.
Acknowledgments
The authors would like to acknowledge all the voluntary donors who donated throughout the pandemic to provide transfusion support to patients with hemoglobin disorders.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Arwa Z. Al-Riyami) for the series “Blood Transfusion during the COVID-19 Pandemic” published in Annals of Blood. The article has undergone external peer review.
Peer Review File: Available at https://aob.amegroups.com/article/view/10.21037/aob-21-53/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aob.amegroups.com/article/view/10.21037/aob-21-53/coif). The series “Blood Transfusion during the COVID-19 Pandemic” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dore B. Covid-19: collateral damage of lockdown in India. BMJ 2020;369:m1711. [Crossref] [PubMed]
- Wang Y, Han W, Pan L, et al. Impact of COVID-19 on blood centres in Zhejiang province China. Vox Sang 2020;115:502-6. [Crossref] [PubMed]
- Bharat S, Rahul K, Indraneel D, et al. Impact of COVID-19 pandemic on the pattern of blood donation and blood safety: Experience from a hospital-based blood center in North India. Asian J Transfus Sci 2021;15:119-24. [Crossref] [PubMed]
- Basavarajegowda A, Bajpai M, Arora S, et al. Survey based cross-sectional study to analyse the variation of practices at blood centres during COVID-19 pandemic in India. Transfus Apher Sci 2021;60:103131. [Crossref] [PubMed]
- Al-Riyami AZ, Abdella YE, Badawi MA, et al. The impact of COVID-19 pandemic on blood supplies and transfusion services in Eastern Mediterranean Region. Transfus Clin Biol 2021;28:16-24. [Crossref] [PubMed]
- Barnes LS, Al-Riyami AZ, Ipe TS, et al. COVID-19 and the impact on blood availability and transfusion practices in low- and middle-income countries. Transfusion 2022;62:336-45. [Crossref] [PubMed]
- Pagano MB, Hess JR, Tsang HC, et al. Prepare to adapt: blood supply and transfusion support during the first 2 weeks of the 2019 novel coronavirus (COVID-19) pandemic affecting Washington State. Transfusion 2020;60:908-11. [Crossref] [PubMed]
- Al-Riyami AZ, Burnouf T, Wood EM, et al. International Society of Blood Transfusion survey of experiences of blood banks and transfusion services during the COVID-19 pandemic. Vox Sang 2022;117:822-30. [Crossref] [PubMed]
- Eleftheriou A, Cannon L, Angastiniotis M. Thalassaemia Prior and Consequent to COVID-19 Pandemic. The Perspective of Thalassaemia International Federation (TIF). Thalass Rep 2020;10:9138.
- Arcot PJ, Kumar K, Mukhopadhyay T, et al. Potential challenges faced by blood bank services during COVID-19 pandemic and their mitigative measures: The Indian scenario. Transfus Apher Sci 2020;59:102877. [Crossref] [PubMed]
- Ranganathan P, Sengar M, Chinnaswamy G, et al. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol 2021;22:970-6. [Crossref] [PubMed]
- Senapati J, Aggarwal M, Louis L, et al. Transfusion practices during the COVID-19 pandemic: An experience from a hematology daycare in India. Transfus Apher Sci 2021;60:103025. [Crossref] [PubMed]
- Iyer S, Sakhare S, Sengupta C, et al. Hemoglobinopathy in India. Clin Chim Acta 2015;444:229-33. [Crossref] [PubMed]
- Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 2008;86:480-7. [Crossref] [PubMed]
- Alsayegh F, Mousa SA. Challenges in the Management of Sickle Cell Disease During SARS-CoV-2 Pandemic. Clin Appl Thromb Hemost 2020;26:1076029620955240. [Crossref] [PubMed]
- Christianson A, Howson CP, Modell B. March of Dimes Global Report on Birth Defects. New York: March of Dimes Birth Defects Foundation, 2006. [Accessed on: 20-05-19].
- Colah R, Italia K, Gorakshakar A. Burden of thalassemia in India: the road map for control. Pediatric Hematology Oncology Journal 2017;2:79-84.
- Colah R, Gorakshakar A, Phanasgaonkar S, et al. Epidemiology of beta-thalassaemia in Western India: mapping the frequencies and mutations in sub-regions of Maharashtra and Gujarat. Br J Haematol 2010;149:739-47. [Crossref] [PubMed]
- Kar S, Seth S, Seth PK. Prevalence of malaria in Ao Nagas and its association with G6PD and HbE. Hum Biol 1992;64:187-97.
- Taylor SM, Parobek CM, Fairhurst RM. Haemoglobinopathies and the clinical epidemiology of malaria: a systematic review and meta-analysis. Lancet Infect Dis 2012;12:457-68. [Crossref] [PubMed]
- CDSCO, Ministry of Health and Family Welfare, Government of India. Regulatory requirements of blood and/or its components including blood products. Available online: https://cdsco.gov.in/opencms/opencms/system/modules/CDSCO.WEB/elements/download_file_division.jsp?num_id=MzY3 [Last accessed on 2020 June 08].
- National Aids Control Organisation, Report on National Estimation of Blood Requirement in India. Available online: http://naco.gov.in/sites/default/files/Final%20Estimation%20Report%20of%20Blood%20Requirement%20in%20India%20%281%29.pdf [Last accessed on 2020 June 08].
- Annual Report 2019-2020, Ministry of Health and Family welfare, Government of India. Accessed 10th August, 2021. Available online: https://main.mohfw.gov.in/sites/default/files/Annual%20Report%202019-2020%20English.pdf
- Singh H, Pradhan M, Singh RL, et al. High frequency of hepatitis B virus infection in patients with beta-thalassemia receiving multiple transfusions. Vox Sang 2003;84:292-9. [Crossref] [PubMed]
- Choudhury N, Phadke S. Transfusion transmitted diseases. Indian J Pediatr 2001;68:951-8. [Crossref] [PubMed]
- Manisha S, Sanjeev K, Seema N, et al. A Cross-Sectional Study on Burden of Hepatitis C, Hepatitis B, HIV and Syphilis in Multi-Transfused Thalassemia Major Patients Reporting to a Government Hospital of Central India. Indian J Hematol Blood Transfus 2015;31:367-73. [Crossref] [PubMed]
- Dhawan HK, Kumawat V, Marwaha N, et al. Alloimmunization and autoimmunization in transfusion dependent thalassemia major patients: Study on 319 patients. Asian J Transfus Sci 2014;8:84-8. [Crossref] [PubMed]
- Elhence P, Solanki A, Verma A. Red blood cell antibodies in thalassemia patients in northern India: risk factors and literature review. Indian J Hematol Blood Transfus 2014;30:301-8. [Crossref] [PubMed]
- Sarnaik S, Schornack J, Lusher JM. The incidence of development of irregular red cell antibodies in patients with sickle cell anemia. Transfusion 1986;26:249-52. [Crossref] [PubMed]
- Aygun B, Padmanabhan S, Paley C, et al. Clinical significance of RBC alloantibodies and autoantibodies in sickle cell patients who received transfusions. Transfusion 2002;42:37-43. [Crossref] [PubMed]
- Gandhi A, Görlinger K, Nair SC, et al. Patient blood management in India - Review of current practices and feasibility of applying appropriate standard of care guidelines. A position paper by an interdisciplinary expert group. J Anaesthesiol Clin Pharmacol 2021;37:3-13. [Crossref] [PubMed]
- Das SS, Biswas RN. Alterations in blood component utilization in a tertiary care hospital in eastern India in the COVID-19 pandemic. Asian J Transfus Sci 2022;16:36-40. [Crossref] [PubMed]
- Enabling Delivery of Essential Health Services during the COVID 19 Outbreak: Guidance note. MOHFW. Available online: https://www.mohfw.gov.in/pdf/EssentialservicesduringCOVID19updated0411201.pdf
- Pandey HC, Coshic P. Blood supply management in times of SARS-CoV-2 pandemic - challenges, strategies adopted, and the lessons learned from the experience of a hospital-based blood centre. Vox Sang 2021;116:497-503. [Crossref] [PubMed]
- Sachdev S, Kishore K, Singh L, et al. Exploration of COVID-19 related fears deterring from blood donation in India. ISBT Sci Ser 2021;16:147-57. [Crossref] [PubMed]
- Radhakrishnan N, Shankar R, Singh S, et al. Taking on a pandemic's challenge: Emergent solutions from a single Hemophlia treatment center in North India. Transfus Apher Sci 2021;60:103022. [Crossref] [PubMed]
- Vilela TS, Braga JAP, Loggetto SR. Hemoglobinopathy and pediatrics in the time of COVID-19. Hematol Transfus Cell Ther 2021;43:87-100. [Crossref] [PubMed]
- Thalassemia International Federation. The COVID-19 pandemic and hemoglobin disorders: a contribution of thalassemia international federation to its global Patientsʼ community (version III, updated). Thalassemia international federation. 2020. Available online: https://thalassaemia.org.cy/wp-content/uploads/2020/03/COVID-19-pandemic-and-haemoglobin-disorders_V3.pdf
- Singh A, Brandow AM, Panepinto JA. COVID-19 in individuals with sickle cell disease/trait compared with other Black individuals. Blood Adv 2021;5:1915-21. [Crossref] [PubMed]
- Haghpanah S, Hosseini-Bensenjan M, Sayadi M, et al. Incidence Rate of COVID-19 Infection in Hemoglobinopathies: A Systematic Review and Meta-analysis. Hemoglobin 2021;45:371-9. [Crossref] [PubMed]
- Karimi M, Mohammadi F, Behmanesh F, et al. Effect of combination therapy of hydroxyurea with l-carnitine and magnesium chloride on hematologic parameters and cardiac function of patients with beta-thalassemia intermedia. Eur J Haematol 2010;84:52-8. [Crossref] [PubMed]
- Cappellini MD, Viprakasit V, Taher AT, et al. A Phase 3 Trial of Luspatercept in Patients with Transfusion-Dependent β-Thalassemia. N Engl J Med 2020;382:1219-31. [Crossref] [PubMed]
- Farmakis D, Giakoumis A, Cannon L, et al. COVID-19 and thalassaemia: A position statement of the Thalassaemia International Federation. Eur J Haematol 2020;105:378-86. [Crossref] [PubMed]
- Uter S, An HH, Linder GE, et al. Measures to reduce red cell use in patients with sickle cell disease requiring red cell exchange during a blood shortage. Blood Adv 2021;5:2586-92. [Crossref] [PubMed]
- Kar R, Dolai TK, Shekhawat PS, et al. Indian Society of Hematology and Blood Transfusion (ISHBT) Consensus Document on Hematological Practice During COVID-19 Pandemic. Indian J Hematol Blood Transfus 2021;37:1-9. [Crossref] [PubMed]
- Menapace LA, Thein SL. COVID-19 and sickle cell disease. Haematologica 2020;105:2501-4. [Crossref] [PubMed]
- Valentino LA, Skinner MW, Pipe SW. The role of telemedicine in the delivery of health care in the COVID-19 pandemic. Haemophilia 2020;26:e230-1. [Crossref] [PubMed]
- Dhiman Y, Patidar GK, Arora S. Covid‐19 pandemic‐response to challenges by blood transfusion services in India: a review report. ISBT Science Series 2020;15:365-73.
Cite this article as: Arora S, Radhakrishnan N, Patidar GK, Dua S. Impact of COVID-19 on transfusion care of patients with hemoglobin disorders in India. Ann Blood 2023;8:15.


