
Impact of the COVID-19 pandemic on blood services operations: Korean experience
Introduction
The coronavirus disease 2019 (COVID-19) outbreak, which was characterized as a pandemic on March 11, 2020 by the WHO, was first reported in December 2019 in Wuhan, Hubei, China (1). In January 20, 2020 the first COVID-19 case in Korea was identified in a Chinese woman, a resident of Wuhan, Hubei province in China (2). A super-spreader linked to a religious group was identified in mid-February in the city of Daegu that led to an explosive outbreak (3). The Korean Disease Control and Prevention Agency (KDCA) responded with the test-trace-isolate strategy implementing enhanced social distancing measures, scaling up of diagnostic capacity, contact tracing using digital technology, and mass screening of thousands of people which contributed to containing the cluster (4). After the super-spreading event in Daegu, waves of clusters in other regions of Korea have been successfully controlled.
The Korean Red Cross Blood Services (KRCBS), responsible for collection, processing and distribution of blood and blood products, covers about 94% of the total transfusion need of the nation. To fulfill this purpose, it operates 15 blood centers, three laboratory centers, one research center and one plasma fractionation center; 142 fixed collection sites and 94 vehicles for blood drives affiliated to the blood centers collect about 2.6 million units of blood donation per year. The COVID-19 pandemic had profound impact on blood supply operations of which blood collections were most affected.
At the time of write up of this manuscript, twenty months into the pandemic, despite strong public health measures and global vaccination efforts, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) still continues to spread across the world. With the emergence of variants, especially the delta variant, Korea is experiencing a fourth wave of COVID-19 infections. This review aims to share measures such as precautionary safety measures to minimize human to human transmission and thus protect both donors and staff, management of donations from donors who are asymptomatic carriers for COVID-19, and measures to balance blood demand and supply taken by the KRCBS. We also aim to discuss the impact of the pandemic on blood services operations.
Precautionary safety measures
During the early stage of the COVID-19 pandemic, the KRCBS responded quickly to adopt public health guidelines enacted by the KDCA. To avoid confusion and anxiety in the community, communicating precautionary safety measures consistent with government guidelines both to prospective donors and staff is of the utmost importance. Messaging posters were posted at every entrance of each donation site to inform prospective donors not to enter if they have fever or respiratory symptoms and how to follow personal hygiene practices. As a four-week deferral policy for overseas travel was already in place before the COVID-19 pandemic, no additional risk mitigation regarding travel was considered to be necessary other than reminding donors not to enter the donation sites if they have a recent travel history. Automatic temperature scanners were installed and hand sanitizers were provided at each donation site to check temperature and keep personal hygiene. Donors and staff were required to wear face masks at all times and masks were also provided to donors appearing without a mask. Donors were advised to arrange donation appointments in advance to reduce waiting time and avoid accompanying people to prevent crowding at donation sites. Signs were posted to keep physical distancing in the reception and refreshment area. Donation sites were disinfected on a daily basis and donation chairs were disinfected after every donation. In addition, monthly disinfection was done by professional cleaning services. Staff members were also requested to self-isolate if they develop COVID-19 related symptoms and seek diagnostic testing if necessary.
Management of COVID-19 related donations
To mitigate the theoretical risk of transfusion-transmission of SARS-CoV-2 via blood donation from pre-symptomatic COVID-19 cases, existing post-donation information policy was enhanced and donors were asked to report any illness or close contact with a confirmed case prior to donation, or being classified as a suspect case or diagnosed as COVID-19 after the donation. Although the importance of post-donation information was emphasized, timely notification before transfusion of the donated products may not occur especially for blood components with a very short shelf life such as platelets. To prevent blood products being transfused at the earliest possible moment and not solely rely on post-donation information provided by the donors, the KRCBS requested to receive the details of all confirmed COVID-19 cases from the KDCA. Starting from March 9, 2020, the KRCBS is receiving the list of all COVID-19 cases identified in Korea and this list is uploaded to the KRCBS’s Blood Information Management System on a daily basis for the purpose of (I) cross referencing to donors for further recipient investigation or (II) recall any blood products not transfused and (III) to apply a three month deferral for donation which has been reduced to a four week deferral on August 4, 2021. With this system in place, we were able to investigate the possible risk of transfusion-transmission of COVID-19 (5). Once COVID-19 cases are identified among the blood donors, repository samples from blood donations of these COVID-19 blood donors are referred to the KDCA for SARS-CoV-2 RNA testing. As of May 2021, 188 cases with confirmed COVID-19 infection were identified among the blood donors. Of these, 93.1% were diagnosed with COVID-19 within three weeks after donation, and 6.9% were diagnosed before donation. The repository samples of these cases, referred to the KCDA, tested negative for SARS-CoV-2 RNA. In total, 538 blood products were prepared from these donations, of which 37% had already been transfused. Among the blood products already transfused 22.1% were platelets, 14.3% red blood cells and 0.6% fresh frozen plasma. All blood products related to the COVID-19 confirmed cases that had not been transfused were recalled and discarded. Patients who had already received the related blood products were reported to the Ministry of Health and Welfare (MoHW), and no case of SARS-CoV-2 transfusion transmission has been identified so far.
Impact on blood collection and blood supply
The COVID-19 pandemic with widespread human to human transmission had a profound impact on blood collection. Donor turnout dramatically decreased because of fear of contracting the virus in public places including donation sites. Blood drives were cancelled because of closing of high-schools, universities and workplaces. The loss of blood donors due to cancellation of blood drives was more pronounced during the COVID-19 pandemic than during the influenza (H1N1) pandemic in 2009 or the Middle East respiratory syndrome (MERS) outbreak in 2015 (Table 1). During the early half of 2020, scheduling of mobile drives to high schools was not possible due to school closure, therefore the actual loss of donors would have been even greater than the data captured for the second half of the year.
Table 1
| Pathogen | Duration | Blood drive sessions | Total, n (%) | High-schools†, n (%) | Military units, n (%) | Other groups, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sessions | Donors | Sessions | Donors | Sessions | Donors | Sessions | Donors | ||||||
| SARS-CoV-2 | January 2020 to December 2020 | Planned | 18,281 | 817,872 | 1,353 | 126,469 | 5,988 | 362,180 | 10,940 | 329,223 | |||
| Cancelled | 804 (4.4) | 51,171 (6.3) | 187 (13.8) | 22,440 (17.7) | 259 (4.3) | 16,835 (4.6) | 358 (3.3) | 11,896 (3.6) | |||||
| MERS-CoV | May 2015 to December 2015 | Planned | 9,202 | 731,541 | 2,436 | 323,289 | 2,614 | 210,840 | 4,152 | 197,412 | |||
| Cancelled | 370 (4.0) | 42,040 (5.7) | 221 (9.1) | 31,090 (9.6) | 46 (1.8) | 3,730 (1.8) | 103 (2.5) | 7,220 (3.7) | |||||
| H1N1 | May 2009 to March 2010 | Planned | 14,688 | 1,074,030 | 2,050 | 281,620 | 4,289 | 432,564 | 8,349 | 359,846 | |||
| Cancelled | 314 (2.1) | 40,590 (3.8) | 172 (8.4) | 27,290 (9.7) | 104 (2.4) | 10,610 (2.5) | 38 (0.5) | 2,690 (0.7) | |||||
†, data for high-schools in 2020 represent data for July 2020 to December 2020. Schools were closed from January to June 2020. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; MERS-CoV, Middle East respiratory syndrome coronavirus; H1N1, influenza A virus subtype H1N1.
In Korea, donors are eligible to donate small volume (320 mL) whole blood if they are 16 years old. To be eligible for other donation types, including large volume (400 mL) whole blood donation or apheresis donation, donors must be 17 years of age or older. Young blood donors (<30 years old) account for more than 65% of the donor population in Korea before the COVID-19 pandemic. However, during the pandemic, and with the delay in high-school and university openings and switch to on-line education, the proportion of young donors among the donor pool decreased to about 56%, resulting in the collection of about 450,000 less units from this age group compared to pre-COVID-19 period (Table 2).
Table 2
| Age, years | 2019 | 2020 | % difference |
|---|---|---|---|
| <20 | 800,321 (28.7%) | 479,602 (19.7%) | −40.1% |
| ≥20 to <30 | 1,017,604 (36.5%) | 889,006 (36.5%) | −12.6% |
| ≥30 to <40 | 431,188 (15.4%) | 413,734 (17.0%) | 4.0% |
| ≥40 to <50 | 358,446 (12.8%) | 410,344 (16.9%) | 14.5% |
| ≥50 to <60 | 155,645 (5.6%) | 206,998 (8.5%) | 33.0% |
| 60–69 years | 27,888 (1.0%) | 35,526 (1.5%) | 27.4% |
| Total | 2,791,092 | 2,435,210 | −12.8% |
Compared to the 2009 H1N1 pandemic and 2015 MERS outbreak, decrease in donor attendance during the COVID-19 pandemic had immediate impact on blood collection and blood inventory levels (Table 3) (6). In the case of the COVID-19 pandemic, it took only 18 days to reduce the inventory level to below 3 days. Korea, being one of the world’s fastest aging societies with a very low birth rate, already had to cope with a decreasing donor pool even before the pandemic. The timing of COVID-19 emergence in Korea (being in the winter, a season of chronic mismatch between demands and supply) and the stringent containment policies that were implemented to control the spread of SARS-CoV-2 only exacerbated the situation (7).
Table 3
| Pathogen | Duration | Number of confirmed cases | Time from disease outbreak to blood shortage† |
|---|---|---|---|
| SARS-CoV-2 | January 2020–ongoing | 195,099 (as of July 28, 2021) | 18 days |
| MERS-CoV | May 2015–December 2015 | 186 | 142 days |
| H1N1 | May 2009–March 2010 | 2,089 | 182 days |
†, blood shortage defined as inventory level of red blood cells of less than 3 days. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; MERS-CoV, Middle East respiratory syndrome coronavirus; H1N1, influenza A virus subtype H1N1.
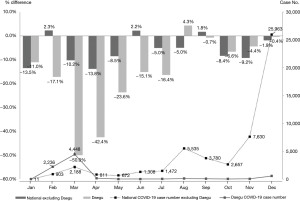
As the initial phase of the pandemic also coincided with the Lunar New Year holidays in early February and was soon followed by the outbreak in the City of Daegu, the epicenter of the COVID-19 outbreak in Korea, blood shortage became only worse. Daegu experienced the most serious impact on blood collection as collections decreased by 40–50% in the months of March and April following the outbreak (Figure 1). This impact persisted for several months and the decrease in donations recovered to national levels only after the second half of the year.
Although a few staff members were diagnosed with COVID-19 disease or were put on quarantine due to close contact with a confirmed case, this did not directly effect blood collection as rescheduling of workforce was able to cover the vacancies.
Measures to manage blood demand and supply
KRCBS worked closely with the government to raise public awareness about the serious impact of the COVID-19 pandemic on blood collection. In collaboration with the MoHW, promotional campaigns on blood donation were broadcasted on mainstream media as well as radio (8-10). Social media postings were not only used to inform the public about the blood shortage but also to clarify misinformation about risks related to blood donation (11).
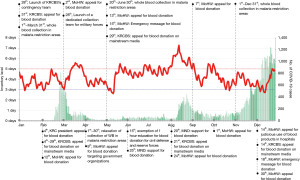
To increase participation of various sectors of the community in blood donation, the KRCBS also collaborated with other government ministries such as the Ministry of Education and the Ministry of National Defense (MND) for school or military participation, respectively. For members of the civil defense and reserve forces participating in blood donation, 1 hour of the mandatory education were exempted. On May and December 2020, the inventory level fell below 3 days. Upon KRCBS’s request, MoHW responded by dispatching national emergency alert messages to the public appealing for blood donation. This resulted in immediate increase in donor attendance leading to increased inventory levels to above 5 days (Figure 2). Although emergency alert messages had a positive impact on blood collection, they should be used judiciously as people might develop a tolerance to these alerts which could undermine their effectiveness.
Korea has geographical restrictions for blood donation with regard to malaria; these restrictions are lifted during the winter season when mosquitoes are not active. Amidst the continuous blood shortage, the Blood Management Committee under the jurisdiction of the MoHW approved the extension of lifting these restrictions until April 2020. After the first relaxation of the restriction, the committee decided to extend the lifting from May 20 to June 30, 2020 with the provision that PCR testing for malaria was performed. The KRCBS quickly set up PCR testing for malaria in May 2020 and was able to collect 14,741 units of whole blood. In 2021, the MoHW again approved collection of donations in these areas from May 1 to June 30, and 8,605 units of whole blood were collected at KRCBS. All donations during these two time periods were tested negative for malaria.
Close collaboration with hospital customers is essential to balance demand and supply and secure blood products for critical need. The Blood Information Sharing System (BISS), was established in 2005 to enable online ordering of blood products and is used to monitor blood inventory levels in hospitals on a daily basis and supply of blood products was adjusted accordingly, thereby avoiding imbalance in blood availability between hospitals. The national inventory level is shared via the KRCBS’s webpage; regional inventory levels were communicated via telephone calls to hospitals. This system proved usefulness during the pandemic to monitor blood demand and supply. Supply of blood products during the first year of the pandemic decreased by 5.2% compared to the previous year due to decreased demand. At hospital level, elective surgeries were postponed or cancelled, use of blood products was triaged and patient blood management practices were emphasized
Collection of COVID-19 convalescent plasma for manufacturing hyperimmune globulin
On May 14, 2020, the MoHW requested KRCBS’s support regarding collection of COVID-19 convalescent plasma (CCP) to support manufacture of hyperimmune globulin co-developed by the Korea Institute of Health (KNIH) and a private domestic pharmaceutical company. Upon this request the KRCBS organized four blood donation drives in the City of Daegu from June 15 to December 4, 2020. From August 24, 2020 to April 30, 2021, CCP was also collected at fixed donation sites in other areas of Korea. Individuals were eligible if three months have passed since their recovery from COVID-19. Other eligibility criteria were the same as for plasmapheresis donors. In total, 3,704 donors participated in the CCP collection. Routine donor screening such as serological and nucleic acid amplification tests for hepatitis B virus, hepatitis C virus, and the human immunodeficiency virus was done at KRCBS’s blood laboratory centers. Testing for anti-SARS-CoV-2 antibodies was organized by the KNIH.
Current and future challenges
On August 11, 2021, daily new COVID-19 cases surpassed 2,000 for the first-time in Korea since the pandemic started. This increase has been attributed to the spread of the Delta variant and also rise in domestic travel during the summer holiday season. Relaxed social distancing restrictions have been raised again to the highest level. A study suggested that at least 62% of the susceptible population needs to be vaccinated to achieve herd immunity in Korea (12). As of August 1, 2021 37.9% of the population eligible for vaccination have received the first dose and 13.9% have received the second dose (13). In early January 2021, the KRCBS requested to the MoHW to include on priority group for vaccination, the staff of the blood services, as essential health care workers. KRCBS’s staff received vaccination starting late April and as of August 1 70.7% received the first dose and 60.9% received the second dose. As vaccination program for those under the age of 30 has commenced in July, vaccination rate is anticipated to increase to above 85% by November. The Korean government’s target is to achieve herd immunity against COVID-19 by November 2021. Despite ramping up vaccination efforts by the government, duration of immunity from vaccination is yet not known and booster shots may be needed for immunocompromised people. Even with herd immunity, end point of SARS-CoV-2 is not in sight and booster vaccines may be needed on a regular basis as are other safety measures. Implications of emerging variants on blood services operations are unclear but are likely to have a negative impact.
Given all these uncertainties with regard to the COVID-19 pandemic, the KRCBS continues to keep close communication with donors, regulators, public health officials, hospitals, and media to respond quickly to changing environment and prepare for the next challenge. Furthermore, in light of the changing demographics caused by the rapidly aging society in Korea, a new paradigm for blood supply management would be required.
Conclusions
The COVID-19 pandemic had an unprecedented impact on the health system. Blood services, an essential part of a health system that relies on the voluntary participation of blood donors, are especially vulnerable to the effect of aggressive measures like social distancing and contact lockdown policies put in place to contain the spread of the virus. Timely adoption of safety measures in line with national guidelines and communicating these policies both to the donors and staff is crucial to avoid confusion and anxiety. To prevent a disruption in the blood supply chain and secure adequate blood inventory levels, concerted efforts of all stakeholders including blood donors, regulators and hospitals is essential.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Arwa Z. Al-Riyami) for the series “Blood Transfusion during the COVID-19 Pandemic” published in Annals of Blood. The article has undergone external peer review.
Peer Review File: https://aob.amegroups.com/article/view/10.21037/aob-21-54/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aob.amegroups.com/article/view/10.21037/aob-21-54/coif). The series “Blood Transfusion during the COVID-19 Pandemic” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- Choi JY. COVID-19 in South Korea. Postgrad Med J 2020;96:399-402. [Crossref] [PubMed]
- Kim SW, Kim SM, Kim YK, et al. Clinical characteristics and outcomes of COVID-19 cohort patients in Daegu metropolitan city outbreak in 2020. J Korean Med Sci 2021;36:e12. [Crossref] [PubMed]
- Kang JH, Jang YY, Kim JH, et al. South Korea’s responses to stop the COVID-19 pandemic. Am J Infect Control. 2020;48:1080-86. [Crossref] [PubMed]
- Kwon SY, Kim EJ, Jung YS, et al. Post-donation COVID-19 identification in blood donors. Vox Sang 2020;115:601-2. [Crossref] [PubMed]
- Kwon SY, Kee EH, Kim HS, et al. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) outbreak in South Korea: risk management at the Korean Red Cross Seoul Nambu Blood Center Vox Sang 2015;109:18. (abstract).
- Abdelrahman Z, Li M, Wang X. Comparative review of SARS-CoV-2, SARS-CoV, MERS-CoV, and influenza A respiratory viruses. Front Immunol 2020;11:552909. [Crossref] [PubMed]
- Ministry of Health and Welfare. COVID-19 blood donation campaign, 2020 [cited August 4, 2021]. Available online: https://youtu.be/syvuMWR7EF0
- Korean Red Cross Blood Services. Blood donation campaign 2020 [cited August 4, 2021]. Available online: https://youtu.be/aTIfTD14M6g.
- Korean Red Cross Blood Services. Blood donation campaign 2020 [cited August 4, 2021]. Available online: https://www.youtube.com/watch?v=wlZEBCFVG4o&list=PLI_z9AuI-AXSTv0ZEREnz1sZPZQBVEJba&index=8.
- Korean Red Cross Blood Services. Blood donation contest prize-winning work 2021 [cited August 4, 2021]. Available online: https://youtu.be/2GIZdTvwIV0.
- Park H, Kim SH. A study on herd immunity of COVID-19 in South Korea: using a stochaistic economic-epidemiological model. Environ Resour Econ 2020;76:665-70. [Crossref] [PubMed]
- Korea Disease Control and Prevention Agency. Korea COVID-19 update (1 August 2021) [cited August 1, 2021]. Available online: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=5741&contSeq=5741&board_id=312&gubun=ALL
Cite this article as: Kwon SY, Cho NS, Jang JS, Song CM, Kim GJ, Kim KJ, Kim DS. Impact of the COVID-19 pandemic on blood services operations: Korean experience. Ann Blood 2023;8:13.


